Cataract is opacities of the lens inside the eye. The human eye has a lens inside it, located behind the iris. The lens is the “zoom” of the eye and it helps focusing the light rays on to the retina.
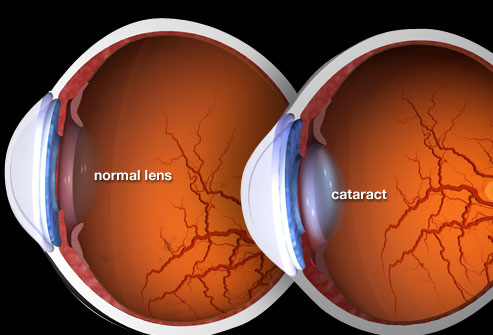
Image from: https://www.webmd.com/eye-health/cataracts/ss/slideshow-cataracts
With age, this lens becomes larger and harder and eventually gets different degrees of opacities. These opacities block some the light rays reaching the retina to different degrees and cause blurred vision. These opacities could be located at the peripheral part of the lens and have minimum effect on vision. On the other hands, they might be located in the central part of the lens and have huge impact on vision despite the limited size of the opacities. The central type of cataract gives often blurred reading vision and glare while driving at night despite having good distance vision. Having said that, the above symptoms are not limited to this type of cataract.
Most of people will develop age-related cataract over the spam of their life. It is thought that the age when age-related cataract might develop is from 40 years old onward, thought the most common age is 60 years old onward.
Symptoms
- Gradual deterioration of vision: distance, reading vision or both. Sometimes people notice that they need more light to see better. Also some patients, find that is becoming more difficult to distinguish colours
- Glare while driving at night or in sunny days
- Double vision or more commonly shadow around things. This usually persist even if you cover the other eye
- Seeing better for reading with the affected eye without glasses: Due to the increased size and hardening of the lens, the cataract could make the affected eye short-sighted and hence make the eye see better for reading without glasses. Over time this usually gets worse. For the same reasons i.e. increase size and hardening of the lens, some patients have to change their glasses more often to keep satisfactory vision.
Causes of cataract
The most common cause of cataract development is age. It is a “natural history” development and all of us at some point will develop cataract but the development of cataract is not an indication for cataract surgery (please see below the indication). There are other causes for cataract development like injury, different medicines side effect and congenital (born with cataract).
Indications for surgery
The indication for cataract surgery is patient’s dissatisfaction with her/his vision enough to justify the small risks of surgery. Nowadays, we do not wait for the cataract to “ripe” nor “until it is ready to be removed”. The technology and techniques of cataract surgery has developed enough to offer surgery when the patient is bothered with his/her cataracts.
There are rare other indications for cataract surgery like helping reducing the intra-ocular pressure in some circumstances, or to balance the refraction (the power of glasses) with the other eye. It is also done for refractive reasons for instance in high short-sighted or long-sighted people who are not willing to wear thick glasses or contact lenses and who are happy to accept the small risks of surgery.
Risks
Like anything in medicine, there are many risks involved in cataract surgery, some of them are insignificant and resolve quickly and others are very serious. I will write in brief the most common risks. For detailed and more information, please read extra literature available widely on the web including different videos.
- During the surgery
- Break in back part of the lens capsule with prolapse of the gel of the eye to the site of surgery. If this occurs the operation will take longer than usual to remove the gel from the front of the eye before an implant can be inserted
- Drop of all or part of the cataract into the back of the If this happen, the patient will need another operation to get it from the back of the eye, usually done by a vitreo-retinal surgeon
- Bleeding inside the eye: This is very rare and I can not re-call seeing one for the last 10 years. If it happens, it can lead to loss of vision
- After the surgery
- High pressure inside the eye: Usually transient and not serious.
- Swelling of the cornea: This is not common and if it happens, it is usually for a short period of time, rarely permanent. Patients with a condition called Fuch’s endothelial dystrophy are at a higher risk of this complication but with the available substances and surgical techniques, even in this category of patients this complication is not common.
- Incorrect strength or dislocation of the implant: If not correctable with suitable glasses it may require a further operation to change or reposition the implant.
- Macular oedema: The macula, is the central part of the retina responsible for central vision. Swelling of the macula occurs in up to 5% of patients but usually transient and clinically in-significant. In 2% of cases, it needs treatment and might delay the full recovery of vision on average but not always for 3 months. The treatment usually is with eye drops and tablets, and minority of patients might need special treatment with injections of steroids.
- Retinal detachment: Very rare, if it happens, will need another surgery and can lead to loss of sight.
- Infection in the eye – endophthalmitis: This is a very serious but rare complication. The current rate of endophthalmitis in the UK is around one in 1000 to 1400 It can lead to loss of sight or even the eye. It requires immediate intensive treatment with injections of antibiotics inside the eye and may require a further operation.
- Allergy to the medication: Redness, itchiness and soreness of the eye, longer than the expected few days for post-operative usual recovery. Usually changing the eye drops is sufficient.
Please, note that the above are the most common but not all possible risks.
Phacoemulsification
Phacoemulsification, is the standard surgery performed for cataract surgery.
- Before the operation:
Before the operation, a nurse or a technician will do some measurements of different parameters of the eye - biometry. These measurements will help the surgeon calculating the power of the intraocular lens (IOL) you will have implanted into your eye after removing your cataract. As mentioned above, the lens in the eye has some refractive power to focus the light rays on to the retina. The IOL which is a lens made from Acrylic material will do the same function as your lens (now called cataract after becoming opaque) that we will remove during cataract surgery i.e. focusing the light rays on to the retina. All modern cataract surgeries include implanting IOLs. The measurements are not always 100% accurate but they will provide you with the best possible power of IOL that suits you. There are different forms of IOL:
Monofocal: These lenses give you the best possible vision for either distance (TV, driving ect), or reading (books and newspapers) or intermediate vision for computers – one particular distance – not all distances.
Toric IOLs: These are the same as monofocal or multifocal IOLs but also correct some irregularities in the shape of the cornea if you have such irregularities.
Multifocal IOLs: Roughly speaking these are like varifocal glasses. They are called premium IOLs because they are expensive. There are many designs of multifocal IOLs. Please check with your surgeon.
Some people choose monovision, i.e. one eye usually the dominant eye sees for distance and the other non-dominant eye sees for reading.
- During the surgery:
The surgery in most of cases is done under local anaesthetic. This includes numbing drops and solution irrigated into the eye. Sometimes, the surgery is done under anaesthetic injection done behind the eye with a blunt tube – this is called sub-Tenon’s anaesthesia. It stops the eye from moving but also stops the eye from seeing for a few hours until the anaesthetic wares off. Rarely, often with medical indication, cataract surgery is done under general anaesthetic.You will go into the operating room walking if you can walk, you will be laid down on the operating table, the eye and surrounding skin cleaned with Iodine solution, a drape placed over your face. The operation is done under the microscope with bright light so you will not see what the surgeon is doing. You might feel some water going on your face, that is normal. The simple straightforward cataract operation takes about 15-20 minutes to do but many cataracts/eyes are not straight forward cases. Some of those cataracts might take longer to carry out safely.
- After the operation:
After the operation, you will be taken walking if you can walk to the post-operative room where you will be given the post-operative instructions and treatment and sent home. The post-operative treatment is usually with eye drops for a few weeks.
A cataract is an opacity or clouding of the natural lens inside the eye. The human eye has a lens inside it, located behind the iris. The lens is the “zoom” of the eye and it helps focusing the light rays onto the retina.
 Image from: https://www.webmd.com/eye-health/cataracts/ss/slideshow-cataracts
Image from: https://www.webmd.com/eye-health/cataracts/ss/slideshow-cataracts
As we age, the natural lens inside the eye gradually becomes larger, harder, and starts to develop varying degrees of opacity. These opacities can block or scatter light entering the eye, leading to blurred vision. If the opacities form at the periphery of the lens, they may have little or no impact on vision. However, when they appear in the central part of the lens, even small opacities can significantly affect vision.
Central cataracts often cause difficulty with reading and glare when driving at night, even if distance vision remains relatively good. That said, these symptoms are not exclusive to central cataracts.
Most people will develop age-related cataracts at some point in their lives. Although cataracts can start forming from the age of 40 onward, they are most commonly diagnosed in individuals aged 60 and above.
Symptoms of cataract
- Gradual deterioration of vision: This can affect distance vision, reading vision, or both. You may notice needing more light to see clearly or find it increasingly difficult to distinguish colours.
- Glare and starbursting: Glare from headlights when driving at night or from bright sunlight during the day is common. Some patients also experience increased sensitivity to light indoors or while watching television.
- Double vision or ghosting: You may notice double vision or a shadow around objects, even when covering the other eye. This symptom often persists and is related to distortion from the cataract.
- Improved near vision in one eye: In some cases, cataracts can cause the affected lens to become more short-sighted. This may temporarily improve your ability to read without glasses in that eye. However, this is usually temporary and tends to worsen over time. As a result, some patients find they need to change their glasses more frequently to maintain clear vision.
Causes of cataract
The most common cause of cataract is age. Cataracts develop naturally as part of the ageing process and almost everyone will develop them eventually. Other causes include eye injury, certain medications, or being born with a cataract (congenital).
Indications for surgery
Cataract
The primary indication for cataract surgery is when a patient’s vision is no longer satisfactory for their daily needs, and they are willing to accept the very small risks associated with surgery. You do not need to wait for a cataract to be “ripe” — modern surgical techniques allow for safe and effective removal of cataracts even in the early stages, provided symptoms are impacting your quality of life.
In some less common cases, cataract surgery may also be recommended for other medical reasons, such as:
- To help reduce intraocular pressure in patients with glaucoma
- To improve refractive balance between the two eyes, particularly when there is a large difference in prescription.
Refractive Lens Exchange (RLE)
Refractive Lens Exchange (RLE) is essentially the same procedure as cataract surgery, but it is performed on a clear (non-opacified) lens. It is offered for refractive purposes, aiming to reduce dependence on glasses or contact lenses. This may be an option for people who are:
- Short-sighted (myopic)
- Long-sighted (hypermetropic)
- Have significant astigmatism
and who prefer a more permanent solution to visual correction.
Different types of intraocular lenses (IOLs) can be used depending on individual needs and preferences. Further explanations about myopia, hypermetropia, and astigmatism are provided below.
How Safe Is Cataract Surgery?
Cataract surgery is one of the most commonly performed and most successful operations in the world, especially when compared to other procedures of similar complexity.
As with any medical procedure, there are risks involved . Most are minor and resolve quickly, but a few — although extremely rare — can be more serious.
While the following section outlines possible complications, it’s important to emphasise that serious problems are very rare, and the vast majority of patients recover well with improved vision.
Possible Complications During Surgery
Although cataract surgery is very safe, complications can occasionally occur during the operation. These are rare and, in most cases, can be effectively managed without affecting the final outcome. Below are some possible complications:
- Tear in the Back of the Lens Capsule (Posterior Capsule Rupture)
This is a break in the thin membrane that holds the lens in place. It can lead to some of the gel (called vitreous) from the back of the eye moving forward. If this happens, the operation will take longer, as the surgeon will need to remove the gel before placing the new lens implant. - Lens Material Falling into the Back of the Eye
Occasionally, part or all of the cataract can drop into the back of the eye. If this occurs, another operation is usually needed to remove the dropped material. This is performed by a specialist eye surgeon called a vitreoretinal surgeon. - Bleeding Inside the Eye (Intraocular Haemorrhage)
This is extremely rare but can occur during surgery. In very rare cases, it may lead to serious vision problems. - Corneal Abrasion
This is a small scratch on the surface of the eye (the cornea), which can happen during surgery. Once the anaesthetic wears off, it may feel sore or gritty. This usually settles within 24–48 hours, and simple pain relief like Paracetamol is often enough to ease any discomfort.
Possible Complications After Surgery
Although cataract surgery is very successful and safe, some complications can occur after the operation. Most of these are temporary and treatable. Serious complications are rare. Here are some possible issues:
- High Pressure Inside the Eye (Ocular Hypertension)
This usually happens temporarily and can be easily treated without causing serious problems. - Swelling of the Cornea (Corneal Edema)
This is uncommon and usually temporary. It may happen more often in patients with very dense cataracts or a condition called Fuchs’ endothelial dystrophy. Even in these cases, modern surgical techniques and materials have reduced the risk significantly. - Incorrect Power or Movement of the Lens Implant
Sometimes the implanted lens may not provide the expected vision correction or may move out of place. If glasses cannot correct the problem, a further operation might be needed to reposition or replace the implant. - Swelling of the Macula (Macular Oedema)
The macula is the central part of the retina that controls sharp vision. Swelling here can occur in up to 5% of patients but is usually mild and unnoticed. About 2% of patients need treatment, which may delay full recovery for around three months. Treatment usually involves eye drops, but occasionally injections into the eye are required. - Retinal Detachment
This is very rare but serious. If it occurs, further surgery will be necessary. - Inflammation of the Iris (Post-operative Anterior Uveitis)
The iris can become inflamed as a reaction to surgery. This is usually controlled with steroid eye drops used for a longer period. - Infection Inside the Eye (Endophthalmitis)
This is a very serious but very rare complication, occurring in about 1 in 1500 cases in the UK. It can cause loss of vision and, in extremely rare cases, loss of the eye. Immediate treatment with antibiotic injections inside the eye and possibly further surgery are required. - Allergic Reaction to Medication
Some patients may experience redness, itchiness, and soreness of the eye or eyelids that lasts longer than expected. Usually, changing the eye drops resolves this. - Clouding of the Lens Capsule (Posterior Capsular Opacification)
In 15–25% of patients, the thin membrane holding the lens implant can become cloudy months or years after surgery. This causes blurred vision similar to a cataract. It can be treated easily with a quick, painless laser procedure called a YAG laser capsulotomy. This restores clear vision in a few minutes. - Visual Phenomena (Dysphotopsia)
Some patients notice unusual visual effects after surgery, such as dark shadows (negative dysphotopsia) or bright arcs or streaks of light (positive dysphotopsia), especially in their peripheral vision. These symptoms are usually mild and improve or disappear within a few months as the brain adapts. In rare cases, if these symptoms persist and cause significant discomfort, further treatment or surgery may be considered.
Please remember: Cataract surgery is a highly successful procedure with a low risk of complications. However, it is important to understand these risks fully, and I will discuss them with you to ensure you can make an informed decision.
Phacoemulsification
Phacoemulsification is the standard surgical technique used in cataract surgery and refractive lens exchange.
Before the Operation
Prior to surgery, a nurse will perform a series of measurements called biometry. These measurements are essential to calculate the correct power of the intraocular lens (IOL) that will replace your natural lens after removal of the cataract or clear lens.
The natural lens of your eye helps focus light onto the retina, enabling clear vision. The IOL, made of high-quality acrylic material, takes over this focusing function after surgery. Implanting an IOL is a routine and standard part of modern cataract surgery.
While biometry is very accurate, it is not perfect. However, it is highly reliable, allowing us to select the best lens power for your eye. My personal success rate in achieving the intended vision outcome is approximately 97%.
Anatomy of the eye
To help you understand your intraocular lens (IOL) options, I’d like to first explain some basic eye anatomy. I’ll keep it as simple and straightforward as possible.
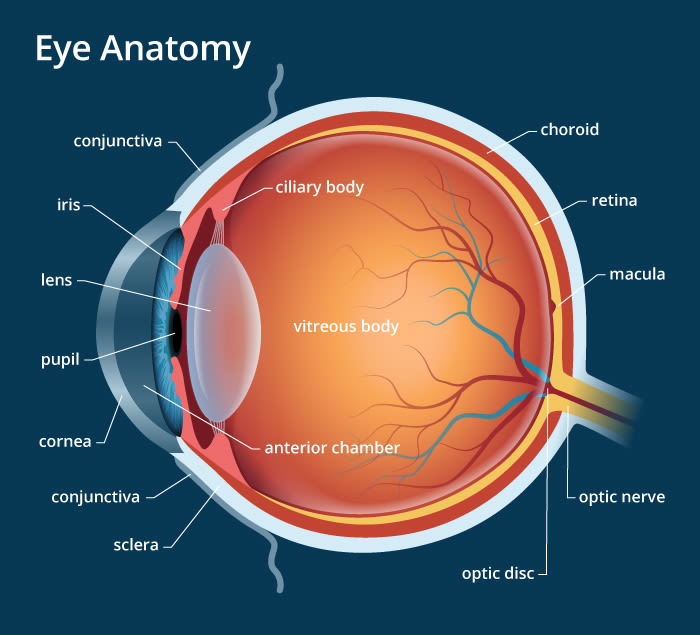
Image from: https://www.allaboutvision.com/resources/anatomy.htm
Learn More About Eye Anatomy
For a better understanding of the anatomy of the eye, you may find it helpful to watch educational videos. One video I often recommend to my patients is available on YouTube: Eye Anatomy Explained
How the Eye Focuses Light
The eye contains two main structures that bend (or refract) light to focus it onto the retina: the cornea and the lens. During cataract surgery or refractive lens exchange, the natural lens is removed and replaced with an artificial intraocular lens (IOL). Because the natural lens is being taken out, we focus our calculations only on the power needed from the IOL—not the original lens.
The cornea, which is the clear, outermost layer at the front of the eye, provides roughly twice the focusing power of the natural lens. Since the shape and refractive power of the cornea, as well as the overall size of the eye, vary slightly from person to person (typically by just a few millimetres), we perform precise, individualised measurements for each eye to determine the correct IOL power.
There are currently over 10 different formulas used to calculate IOL power, highlighting that no single method is perfect for every case. Your surgeon will choose the most suitable approach based on your specific eye measurements.
Refractive errors of the eye
You can watch a helpful video from the American Academy of Ophthalmology that explains the different types of refractive errors in simple terms, using clear language and easy-to-follow illustrations:
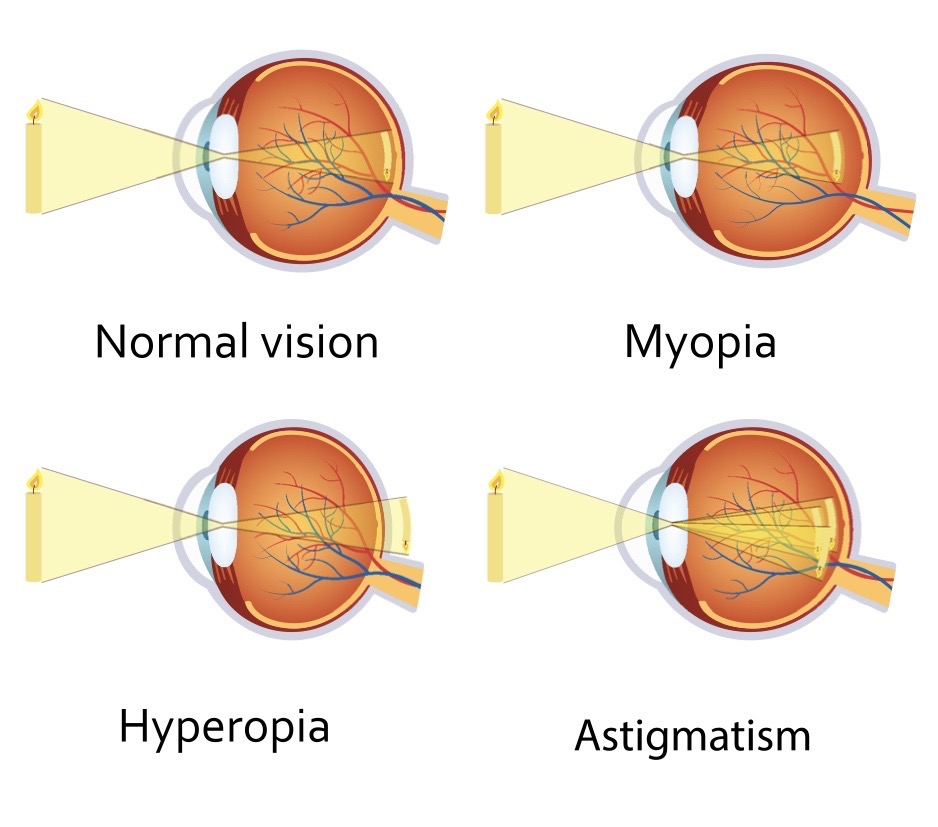 Image from: https://bhtoptometry.com/eye-care/myopia-control/
Image from: https://bhtoptometry.com/eye-care/myopia-control/
Myopia, or short-sightedness, occurs when the combined refractive power of the cornea and lens is too strong for the length of the eye. As a result, images focus in front of the retina instead of directly on it. This causes distant objects to appear blurry, while near objects may still be seen clearly. In cases of moderate to high myopia, patients often need glasses for both distance and reading to properly correct their vision.
Hypermetropia, or long-sightedness, occurs when the combined refractive power of the cornea and lens is too weak for the length of the eye, causing images to focus behind the retina (the opposite of myopia). In mild cases, younger people can often compensate by using the eye’s natural focusing ability. However, as this focusing power decreases with age, they typically need reading glasses first, and later glasses for distance as well. In moderate to high cases, glasses are usually required much earlier, often starting in childhood.
Astigmatism, In both myopia and hypermetropia, we often assume the cornea is perfectly spherical, meaning all its meridians refract light with the same power. However, in reality, this is not the case. About 30% of people have more than 1.0 diopter (unit of measurement) of variation in refractive power across different meridians of their cornea—this is called astigmatism. Astigmatism causes light to focus at multiple points—either in front of, behind, or on the retina—instead of a single clear focus, leading to blurred or distorted vision.
All the above conditions are usually corrected with glasses, contact lenses or surgery.
Types of intra-ocular lenses (IOLs):
- Monofocal IOLs with mild focus extension (I use Eyhance from Johnson & Johnson) give the best possible vision for one distance chosen by the patient but patients will need glasses for other distances. For example, if the patient chooses to see well for distance without glasses, then she/he will need glasses for reading newspapers and computer screen. Or, if the patient chooses to read without glasses for near (books and mobile phones), then she/he will need distance glasses and so on. Having said the above, it is difficult to give 100% guarantee of glasses free vision in all cases. Some patients will need small refinement prescription glasses for the chosen option as well, especially when they have a pre-existing astigmatism in their cornea, unless they chose a monofocal toric IOL to correct it. Please, discuss with me your particular case
Some people choose mono-vision or mini-mono-vision with monofocal IOLs to reduce their dependence on glasses. If there is astigmatism, then this needs to be corrected as well with a toric IOL.
In the full mono-vision The dominant eye is set for clear distance vision without glasses, while the non-dominant eye is focused for near tasks like reading. Many patients who have experience with this type of vision through glasses or contact lenses, know what to expect.
In the mini-mono-vision The dominant eye is set for distance vision, while the non-dominant eye provides better intermediate vision (for activities such as computer use or viewing a car dashboard) without glasses. If you find this unsatisfactory, glasses can still be used for distance and reading.
- Multifocal IOLs provide reasonable vision without glasses for distance (like driving and watching TV), intermediate (like the computer screen or the car’s dashboard)) and close reading (like the newspaper, books or the mobile phone). There are many designs in the market.
A small number of patients with multifocal IOLs may experience some difficulties, such as reading in dim light, where reading glasses can help. Some patients also notice halos or glare around lights when driving at night. Fortunately, in most cases, the brain gradually adapts to these visual effects over time, making them less noticeable.
Choosing multifocal IOLs involves a trade-off: you may accept some loss in visual quality (such as glare or halos in bright or night time conditions) in exchange for greater freedom from glasses for both distance and near vision.
For patients seeking perfect, flawless vision, I usually do not recommend multifocal IOLs. However, for those willing to accept this trade-off, satisfaction rates are very high. Most of my patients with multifocal lenses are extremely happy with their vision within weeks, and occasionally it may take a few months to fully adapt.
Although rare, in some cases a multifocal IOL may need to be removed and replaced with a monofocal IOL if the patient is dissatisfied. This is very uncommon when thorough pre-surgery evaluations and clear discussions about expectations have taken place.
I use two types of multifocal IOLs: The Galaxy from Rayner (a UK-based company) and the Odyssey from Johnson & Johnson.
The Galaxy lens is one of the first artificial intelligence-designed implants. Instead of the traditional concentric rings, it features a spiral transition of different refractive zones. This design has significantly reduced glare and halos commonly seen with multifocal IOLs, although it has not eliminated them completely. So far, my patients have given very positive feedback.
The Odyssey is an advanced multifocal IOL that also reduces glare and halos by smoothing the transitions between refractive zones more effectively.
During your consultation, I will discuss which implant is the best option for you.
-
Extended depth of focus IOLs (EDOF IOL) I use the PureSee IOLs from Johnson & Johnson, which are among the best in this category. These lenses provide excellent distance vision (such as for driving and watching TV) and intermediate vision (like reading a computer screen or seeing the dashboard) with significantly less glare compared to multifocal IOLs, as they do not have rings in their design. However, patients may still require glasses for close-up reading (books, mobile phones, newspapers), especially in dim lighting.
In some cases, we can improve near vision by intentionally leaving the non-dominant eye slightly short-sighted, a technique called mini mono-vision. This allows that eye to see better for close reading without glasses, though its distance vision will be slightly less sharp compared to the dominant eye. Occasionally, patients may still choose to wear glasses for tasks requiring very clear vision, such as reading small print or reading in low light. Please discuss this option with me during or after your consultation.
One advantage of PureSee EDOF IOLs is that they can be used in eyes with other eye conditions such as macular degeneration, glaucoma, or diabetic retinopathy. Multifocal lenses are generally not recommended for patients with these conditions, but EDOF lenses can be safely implanted alongside other eye diseases.
As always, while we aim for glasses-free vision, I cannot guarantee 100% independence from glasses in every case. I will explain all available options in detail during your consultation.
- Toric IOLs Toric intraocular lenses (IOLs) are available in monofocal, extended depth of focus (EDOF), and multifocal options to correct astigmatism in the eye. If you opt for an EDOF or multifocal IOL, correcting astigmatism with a toric version is essential to achieve the best possible vision without glasses.
Toric lenses must stay precisely aligned within the capsular bag to function correctly. In rare cases, the IOL may rotate slightly after surgery—typically within the first 24 hours. If this occurs, a simple procedure can be done to reposition the lens correctly.
Choosing the right intraocular lens is not always straightforward and should involve a thorough discussion with your surgeon. Please also note that Toric, EDOF, and Multifocal lenses are custom-order implants, so Spire Hospital requires 7–10 days to receive them once ordered.
The Operation
Prior to surgery, a small pellet will be placed into the eye to gently enlarge the pupil. In most cases, the procedure is performed under local anaesthesia. This involves using numbing eye drops and an anaesthetic solution irrigated into the eye.
Occasionally, an injection of anaesthetic is given behind the eye using a blunt cannula (not a needle)—this is called sub-Tenon’s anaesthesia. It temporarily prevents eye movement and vision for a few hours until the anaesthetic wears off. In certain cases, patients may prefer to have the surgery under general anaesthesia.
You will walk into the operating theatre if you are able to, and then lie down on the operating table. The area around your eye will be cleaned with an iodine solution, and a sterile drape will be placed over your face. The operation is performed under a microscope with a bright light, so although you’ll see light, you won’t see the surgeon’s instruments or movements.
During the surgery, you’ll be asked to keep your head still and lie as flat as possible. We will ensure you’re comfortable before the procedure begins. A nurse will hold your hand throughout the operation—if you need to communicate, simply squeeze their hand.
You may feel some water on your face during the procedure; this is completely normal. A straightforward cataract or refractive lens exchange operation typically takes 15–20 minutes, but more complex cases may take longer to complete safely.
At the end of the procedure, a clear plastic shield will be placed over the eye to protect it during the first night after surgery.
After the operation:
Following the surgery, you will be helped back to your room—walking if you are able. There, you’ll be offered a light meal and a hot drink. You will also receive post-operative instructions and your eye drop medication, which you’ll need to use for several weeks after surgery. Once everything is explained and you feel ready, you’ll be discharged home the same day.
The morning after the operation:
You may remove the eye shield the day after surgery. If your eyelids feel sticky, gently clean them using cooled, boiled water and a clean tissue or cotton pad—always wash your hands first. Avoid rubbing your eye, especially in the first few days.
I recommend wearing the plastic eye shield over your operated eye when you go to bed for the first 7 nights after surgery to protect it while you sleep
It is normal to feel some mild discomfort or grittiness following the operation. Over-the-counter lubricating drops can help ease these symptoms.
You can begin using your prescribed eye drops as instructed once the shield is removed.
Most daily activities can be resumed the day after surgery. You may bend gently and lift light objects. Sports and swimming should be avoided for 4 weeks.
You may return to work when you feel comfortable. If your job involves heavy lifting or a dusty environment, please allow 2–3 weeks before resuming those duties.
You can shower and wash your hair the day after surgery, but try to keep water, soap, shampoo, hair spray, and shaving products away from your eye—especially during the first week.
You may drive once you are able to clearly read a vehicle’s registration plate from 20.5 meters and do not have any other eye conditions (such as glaucoma) affecting your visual field. If you have any concerns or known co-existing eye conditions, please check with me before resuming driving.
Full healing usually takes about 4 weeks. After this period, your optician can check your vision and prescribe new glasses if needed.